Uterine fibroids are a common and generally benign condition that many women experience, especially during their reproductive years. According to the Menopause Journal, 70%–80% of women will experience fibroids at least once in their life.(1)
The female hormones estrogen and progesterone significantly contribute to the growth of uterine fibroids. As these hormones decline during menopause, fibroids may shrink. However, in some cases, fibroids can continue to grow during menopause.
Fibroids can cause a variety of symptoms, ranging from severe cramps to heavy bleeding, with some women experiencing no symptoms at all. It’s important for all affected women to consult a physician and manage their symptoms to enjoy a better quality of life during the menopause transition.
What are uterine fibroids?
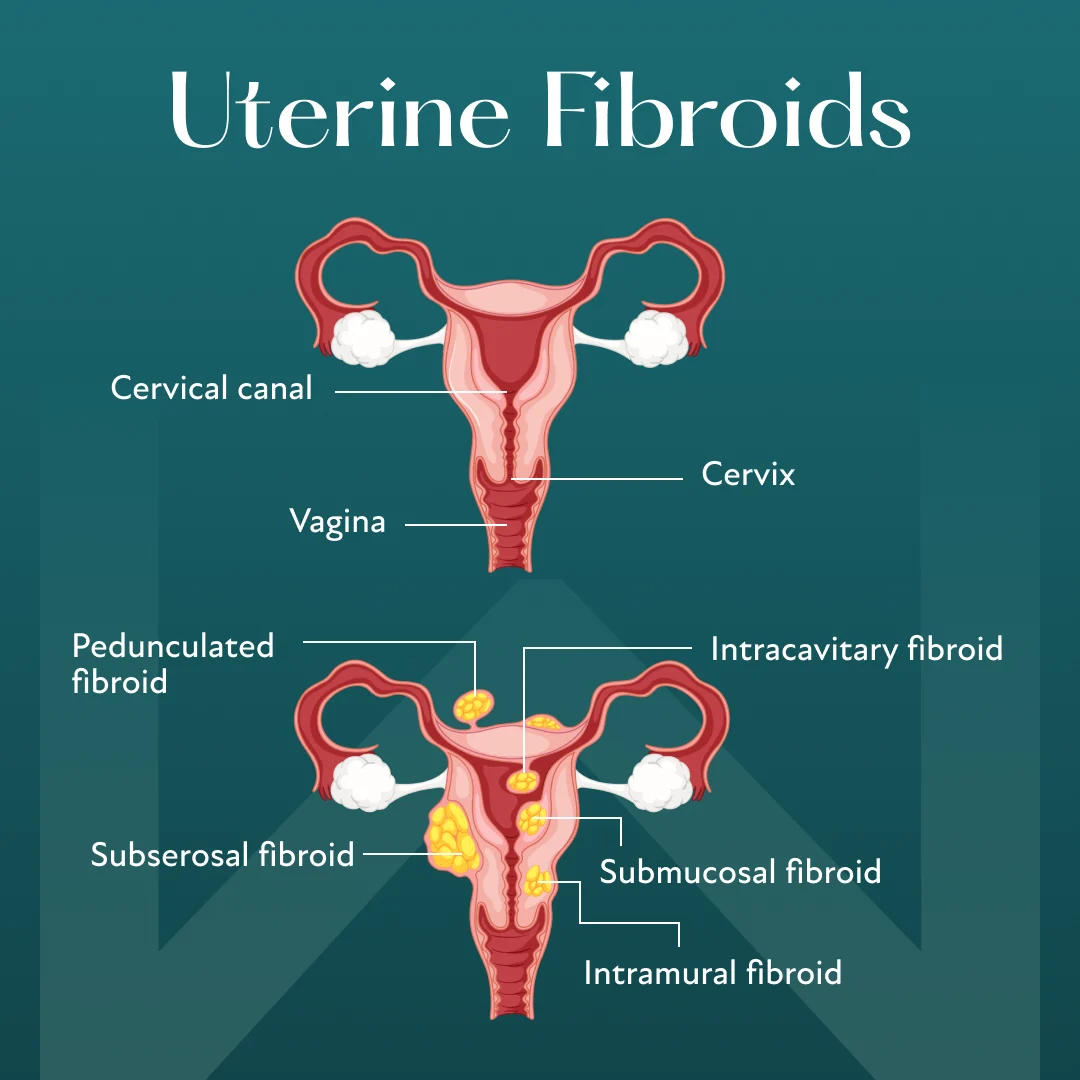
Uterine fibroids are benign overgrowths that develop on the wall of the uterus. They vary in shape and size and appear as a single tumor or multiple growths.(2) Fibroids can occur in the inner lining, the surrounding muscle layer, or the outer surface of the uterus.
Causes of Uterine Fibroids
While the exact cause of fibroids is not known, researchers believe that the following factors may play a role:(3)(4)(5)
Hormones
Uterine fibroids thrive on estrogen and progesterone. Studies suggest fibroids have more receptors for these female hormones than the adjacent uterine tissue. Thus, higher levels of estrogen or progesterone may contribute to the development and growth of uterine fibroids.
Genes
Some fibroids may develop due to inherited genetic mutations. Mutated genes can change how uterine cells divide and multiply, resulting in overgrowth.
Obesity
A 2015 study showed that obesity may increase the risk of uterine fibroids by 46%.(4) The adrenal glands produce androgen precursors, which can be converted to estrogen in fat tissue. Fat tissue may also be more efficient at converting the hormone androstenedione to estrone, a type of estrogen. These factors may increase estrogen levels, a major contributor to the development of uterine fibroids.
Other Factors
In addition to the causes mentioned above, several other factors may also increase the risk of developing uterine fibroids:(3)
Ethnicity: Black and brown women may be more prone to fibroids than white women.
Vitamin D deficiency: Low levels of vitamin D are commonly found in individuals with uterine fibroids, indicating that a deficiency in this vitamin may play a role in fibroid development.
Hypertension: Individuals with high blood pressure can be five times more likely to develop uterine fibroids compared to those with controlled blood pressure.
Pregnancy: Women who have never been pregnant may be at a higher risk of developing uterine fibroids than those who have had one or more pregnancies.
Dietary factors: Some studies suggest that frequent consumption of food additives, red meat, or soybean milk may increase the risk of uterine fibroids.
Symptoms of Uterine Fibroids During Menopause
Each woman's experience with uterine fibroids during menopause can vary. While some women may experience mild symptoms, others might suffer from more severe symptoms that can significantly impact their ability to perform daily activities.
Approximately half of women affected by uterine fibroids don’t experience any symptoms at all.(1) In such cases, fibroids are often discovered incidentally during diagnostic tests like ultrasounds for other purposes.
When present, common symptoms of uterine fibroids during menopause can include the following:(1)(2)
Pelvic pain or a feeling of fullness
Prolonged or heavy menstrual bleeding
Frequent urination
Back or leg pain
Unexplained weight gain
Uterine Fibroids and Menopause
Declining levels of female hormones during menopause may cause fibroids to shrink. Smaller fibroids usually don't cause any symptoms. However, in some women, fibroids may continue to grow even after menopause. In such cases, women might experience symptoms such as abdominal cramps and abnormal bleeding.
Uterine Fibroids in Perimenopause
A 2021 journal review revealed that 30% of women may develop a uterine fibroid for the first time between the ages of 45 and 49, which often coincides with perimenopause.(1)
The approach to managing uterine fibroids during perimenopause depends on the severity of the symptoms. A physician may recommend watchful waiting for women with no symptoms or mild symptoms. If symptoms are severe and impact a woman’s quality of life, medical or surgical options may be considered.
Uterine Fibroids in Postmenopausal Women
Uterine fibroids typically shrink after menopause in most women. However, factors such as race, weight, or genetics may cause them to continue growing even after menopause.(1) The treatment approach for uterine fibroids in postmenopausal women follows a similar strategy to that used during perimenopause.
Treatment Options for Uterine Fibroids After Menopause
As fibroids tend to stop growing or grow more slowly after menopause, a physician might recommend watchful waiting if the symptoms are mild. However, other treatment methods may be necessary for women who have severe symptoms or whose fibroids continue to grow even after menopause. Some effective approaches include the following:
Watchful Waiting
Asymptomatic fibroids typically don’t require treatment. However, women may need to undergo regular tests like pelvic examinations and ultrasounds to monitor the growth of the fibroids.
Medications
Medicines may reduce heavy bleeding or cramps associated with fibroids. Treatment with medications may include the following options:(1)
Tibolone: This is a synthetic hormone with mild estrogenic and progestogenic effects. Studies have shown that tibolone can improve abnormal bleeding and other menopausal symptoms without increasing the size of the fibroids, making it a viable alternative to hormone replacement therapy (HRT).
Aromatase inhibitors: These medicines may help lower estrogen levels in the body, potentially reducing fibroid-related symptoms.
Selective estrogen receptor modulators (SERMs): Studies suggest that these medicines may help suppress the growth of fibroids and even reduce their size in postmenopausal women.
Selective progesterone receptor modulators: These medicines may also help reduce fibroid size, manage fibroid-related symptoms, and improve quality of life.
Gonadotropin-releasing hormone (GnRH) agonists: They can stop the menstrual cycle and reduce fibroid size in some cases.
Minimally Invasive Procedures
A common and effective procedure for fibroid treatment is uterine artery embolization (UAE). This radiologic technique blocks the uterine arteries to reduce blood flow to the uterus and fibroids. UAE has a success rate of 88% in improving uterine fibroid symptoms.(1) It’s a good alternative to hysterectomy for women who wish to preserve their uterus.
Radiofrequency ablation (RFA) is another minimally invasive procedure that uses heat and energy to shrink the fibroids.
Surgery
Myomectomy is a surgical procedure to remove fibroids while leaving the uterus in place. It’s a preferred treatment for multiple or large uterine fibroids. In some cases, fibroids may grow back after a myomectomy.(1)
Hysterectomy is the surgical removal of the uterus, and the ovaries may or may not be removed. This procedure is often recommended for women with recurrent or multiple fibroids.
HRT and Uterine Fibroids After Menopause
HRT may be an effective treatment method for managing uterine fibroids in some women, especially if they are also experiencing menopausal symptoms like hot flashes or joint pain. Anyone considering HRT for their fibroids should speak with a physician who can help determine if it’s the right option for them.
Living With Uterine Fibroids
An individual’s experience living with uterine fibroids depends largely on the severity of the symptoms. Severe cramps, heavy bleeding, and fatigue can affect their ability to perform day-to-day activities.
Women need to know that treatment options are available regardless of symptom severity. Consulting a physician ensures they receive the best possible care and can transition through menopause with greater ease.
When to See a Doctor
While individuals affected by uterine fibroids should seek medical help, the presence of the following symptoms may indicate a worsening condition that requires immediate consultation with a doctor:(6)
Heavy periods
Severe cramps
Sharp, sudden abdominal pain
Lightheadedness
Extreme fatigue
Experiencing menopausal uterine fibroids? Discover if HRT is right for you.
If you’ve entered the menopause transition and are struggling with uterine fibroids, you don’t have to suffer in silence. Take our brief menopause quiz to see if you’re an eligible candidate for HRT. Get started with Winona to take the first step toward feeling better.