Occasional indigestion is a common symptom for many adults. However, some women may experience frequent or severe digestion problems during menopause. In a comparative study, 42% of women going through the menopausal transition reported experiencing upper abdominal discomfort, which is a common indicator of indigestion.(1)
Individuals experiencing indigestion should consult a doctor who can suggest appropriate treatment methods. Managing indigestion can help prevent potential complications, such as stomach ulcers. It also improves quality of life and helps women navigate the menopause transition with more ease.
What is indigestion?
Indigestion, also known as dyspepsia, is a symptom characterized by discomfort in the upper abdominal area. Individuals experiencing indigestion may describe this discomfort as bloating, fullness, or pain after a meal.(2)
Dyspepsia can sometimes be confused with heartburn, which is also a common occurrence during menopause. While heartburn is marked by a burning sensation, indigestion may involve a range of sensations in the upper abdomen.
What are the symptoms of indigestion?
Indigestion can encompass a variety of symptoms, including the following:(3)
Bloating
Burping
Discomfort or burning in the upper abdomen after a meal
Feeling full too soon after a meal
Gurgling in the stomach
Flatulence
Regurgitation of liquid or food
How can menopause increase the risk of indigestion?
Various changes happening in the body during menopause may contribute to indigestion:
Decreased Estrogen
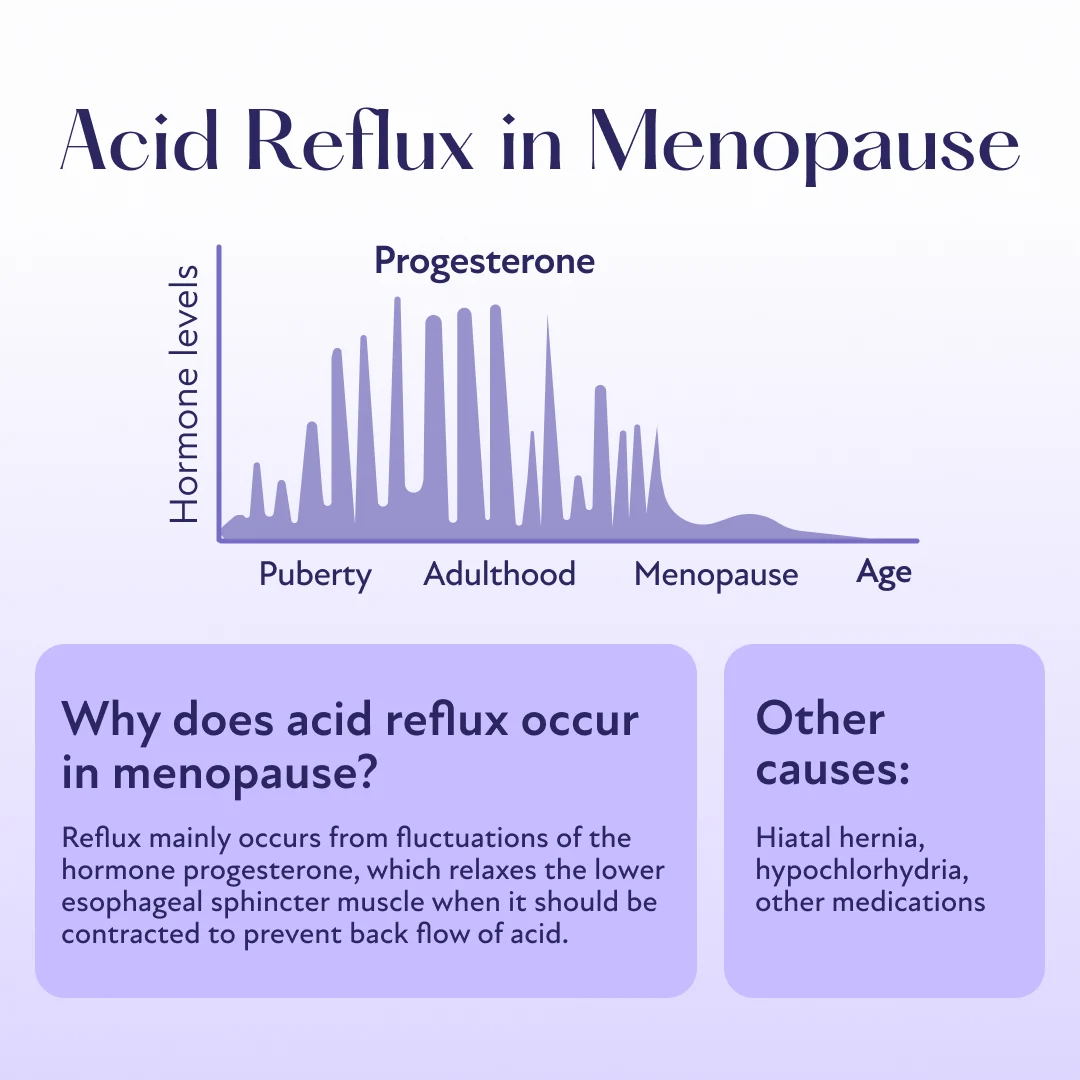
The esophagus, or food pipe, has contractile muscles called sphincters at both ends. The lower esophageal sphincter prevents the entry of food and other substances from the stomach into the esophagus and vice versa.
Estrogen plays a role in maintaining the strength of these sphincters. With declining estrogen levels during menopause, the lower esophageal sphincter may weaken and allow stomach acid to enter the food pipe. This condition is known as gastroesophageal reflux disease (GERD), which may cause inflammation or irritation of the esophageal lining, resulting in symptoms such as heartburn, chest pain, and indigestion.
Estrogen may also help strengthen the bonds between the cells that make up the lining of the gut. These cells, along with the mucosal cells, protect the food pipe from GERD-associated injury. As estrogen levels decrease during menopause, the integrity of these cells may be compromised. This can make the food pipe more vulnerable to GERD-related injury and result in symptoms like indigestion.(4,5)
Slowed Digestion
Abnormal estrogen and progesterone levels can slow down digestion, delaying the emptying of food from the gut. This can cause nausea, bloating, and a sensation of fullness in the abdomen.(6)
Increased Stress
Menopause often coincides with stressful life events such as children leaving home, caring for aging parents, career shifts, and relationship changes like divorce or widowhood.
Studies suggest that stress may affect the gut-brain axis, which carries signals between the gut and the brain. The gut-brain axis involves chemicals that regulate mood, the nervous system, and the gut microbiome.(7)
The gut microbiome refers to the community of microorganisms living in the digestive tract, including bacteria, viruses, and fungi. A healthy gut microbiome is essential for normal digestion, nutrient absorption, and overall gut health. However, stress can disrupt the balance of these microorganisms, potentially leading to indigestion and other digestive issues.
Other Potential Causes of Indigestion
While menopause may cause indigestion in some women, certain factors can further increase this risk, including the following:(3)
Diet and Lifestyle
Eating habits can influence the strength of the gut lining. The following factors may damage the gut lining or disrupt the digestive process, leading to indigestion during menopause:
Drinking too much alcohol, coffee, or caffeinated and carbonated drinks
Eating too quickly
Consuming spicy, fatty, greasy, or acidic foods
Smoking
Medications
Indigestion can be a side effect of some medicines:
Certain antibiotics like tetracycline and clindamycin
Nonsteroidal anti-inflammatory drugs (NSAIDs) like aspirin and ibuprofen
Nutritional supplements like iron and potassium
Health Problems and Digestive Conditions
The following health conditions may cause indigestion as an associated symptom:
Gallbladder inflammation
Gastritis
Irritable bowel syndrome (IBS)
Lactose intolerance
Peptic ulcer disease
Diagnosing Indigestion During Menopause
While occasional indigestion may be a common symptom during menopause, persistent or severe signs can indicate a worsening condition. In such cases, women should consult a physician who can diagnose the underlying cause and suggest appropriate treatment methods.
Treating Indigestion During Menopause
Unhealthy dietary or lifestyle choices may increase the risk of indigestion during menopause. Conversely, adopting a healthy diet and staying active can improve digestion.
Dietary Modifications
Experts recommend these dietary habits to improve digestion:
Avoiding carbonated drinks, coffee, and alcohol
Eating small amounts of food slowly during meals
Opting for low-fat food items such as egg whites, lean meats, and legumes
Consuming high-fiber foods like fruits, vegetables, whole grains, nuts, and seeds
Drinking at least eight glasses of water daily
Lifestyle Changes
The following lifestyle choices can support healthy digestion:
Getting at least 30 minutes of moderate-intensity exercise, such as jogging, running, or swimming, five days a week
Trying relaxation techniques like yoga, meditation, and deep breathing exercises to manage stress
Getting at least eight hours of uninterrupted sleep
Quitting smoking
Medications
Pharmacological interventions that may help manage indigestion include over-the-counter (OTC) and prescription medications.
OTC medicines:(8)
Antacids: They neutralize stomach acid, which is a major contributor to GERD-related gut injury.
Acid reducers: Two types of medications can reduce stomach acid production: histamine antagonists (H2 antagonists) and proton pump inhibitors (PPIs). Cimetidine and famotidine are some OTC H2 antagonists. Common OTC PPIs are esomeprazole and omeprazole.
Combination antacid/acid reducer: These medications combine the acid-neutralizing effects of antacids with the acid-reducing actions of PPIs and H2 blockers.
Prescription medicines:
H2 Blockers and PPIs: These medicines work similarly to their OTC counterparts but are available in higher doses. A physician may prescribe these if OTC medicines don’t provide adequate relief from indigestion. Famotidine and cimetidine can be obtained OTC or by prescription, depending on the dose. Lansoprazole and omeprazole are PPIs available by prescription in stronger concentrations.
Promotility agents: They enhance the movement of the gut and prevent acid from remaining in the stomach for too long. A common example of promotility medication is metoclopramide.
Hormone Replacement Therapy (HRT)
Declining hormone levels during menopause are a major contributor to the gut changes responsible for indigestion. HRT can help prevent this risk by providing these hormones supplementally.
Studies have demonstrated the benefits of HRT in managing anxiety, hot flashes, and other menopausal symptoms, which can increase the risk of indigestion during menopause.
When to See a Doctor for Indigestion
Severe or frequent indigestion may be an indicator of a more serious problem. Women experiencing the following symptoms should consult a doctor immediately:(3)
Blood in vomit
Frequent vomiting
Black stools
Loss of appetite
Difficulty swallowing
Pain radiating to the neck, arm, or jaw
Shortness of breath
Experiencing menopausal indigestion? Discover if HRT is right for you.
If you’ve entered the menopause transition and are struggling with indigestion, you don’t have to suffer in silence. Take our brief menopause quiz to see if you’re an eligible candidate for HRT. Get started with Winona to take the first step toward feeling better.