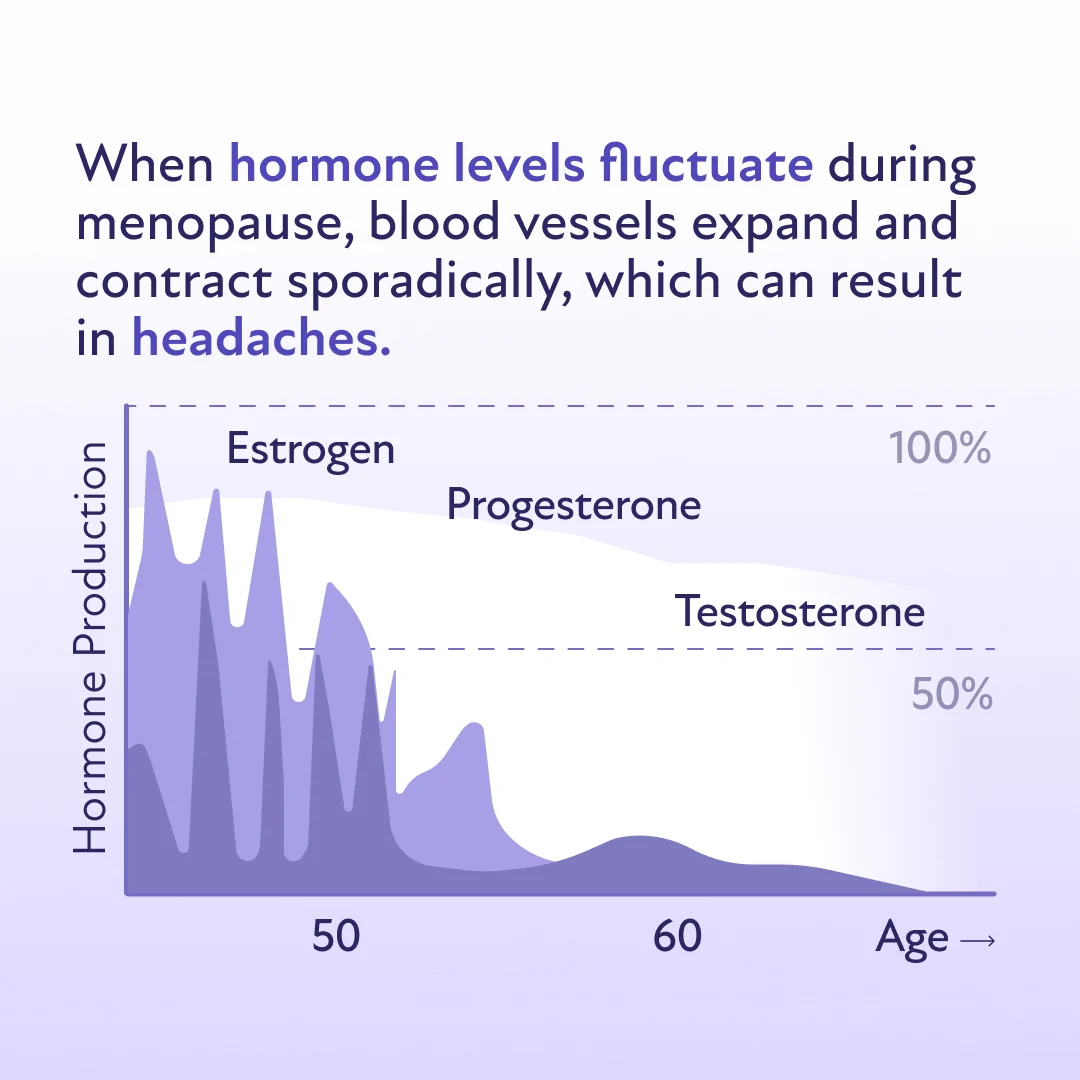
Headaches, including migraines, are a prevalent concern among adults, particularly women undergoing the menopausal transition. Research indicates that stable estrogen levels may reduce headaches, whereas sudden changes can intensify them. Some women may experience fewer headaches during menopause, while others may have it worse.
The prevalence of migraines during menopause is reported to be between 10% and 29%. The impact of these migraine episodes is profound, with 80% of women experiencing more than one episode a month and 75% suffering from severe pain.(1)
However, women are not helpless against these headaches caused by hormonal shifts. Effective treatment options are available, including hormone replacement therapy (HRT), pain relievers, and lifestyle modifications. Healthcare providers can guide women in choosing the most effective approach to treat or prevent hormone-related headaches tailored to their specific needs or issues.
Are headaches and migraines more common during menopause?
As women approach menopause, some may experience an increase in the frequency and severity of headaches and migraines. Even though menopause symptoms can vary for different individuals.
A study found that some women may have experienced migraines for the first time in the years leading up to menopause, while others noted that their headaches became less frequent and less severe. (1,2)
In addition, women who have undergone surgical menopause often face more significant challenges with migraines than those who go through natural menopause.(1,2)
Why do headaches and migraines increase during menopause?
The relationship between menopause and headaches is complex, involving brain chemicals, pain pathways, and vascular systems.
Ovarian steroids, like estrogen, can cross the blood-brain barrier, resulting in their levels in the brain being similar to those in the blood. Specific areas of the brain linked to pain perception have receptors sensitive to estrogen. As estrogen levels drop during menopause, these receptors become more sensitive to pain. This increased sensitivity can lead to headaches and migraines becoming more frequent or severe.(1,2)
Estrogen also interacts with various brain chemicals and systems linked to migraine. For instance, estrogen influences the serotonergic system, which regulates pain and mood.
It also affects the glutaminergic system, which enhances nerve cell activity, as well as other neurotransmitters such as norepinephrine, dopamine, and endorphins. These changes can impact the brain's networks that process pain and the blood vessel system, contributing to the development of migraine symptoms.(1,2)
Types of Headaches During Menopause
Women may experience various types of headaches during menopause:(3,4)
Migraines
Migraines are moderate to severe headaches characterized by throbbing or pulsating pain that intensifies with physical activity. They are commonly associated with heightened sensitivity to sound and light.
Women may experience either of the following migraine variants:
Migraine with aura: This involves visual and sensory disturbances that precede the pain. These disturbances can include seeing spots, geometric patterns, or flashes of light and experiencing numbness or tingling in the limbs or face, limb weakness, or speech difficulties. Some individuals may also report hearing noises or music that are not there.
Migraine without aura: This is the more common type that involves migraine pain without these sensory disturbances.
Tension Headaches
Tension headaches typically present as a dull, continuous ache around the head and scalp. These headaches, often caused by stress and muscle tension, create a sensation of tightness and squeezing in the skull, which contrasts with the pulsating nature of migraines. They are usually mild to moderate in severity and do not typically accompany sensitivity to light or sound or cause nausea.
Cluster Headaches
Cluster headaches are excruciating and typically occur in cyclical patterns or clusters. These episodes can be so severe that they awaken individuals from sleep. Characterized by intense, piercing pain, cluster headaches usually focus around or behind one eye and are confined to one side of the head. The pain from a cluster headache is often described as sharp with a burning sensation.
Other Triggers for Headaches and Migraines During Menopause
In addition to hormonal changes, several other factors can exacerbate or initiate headaches and migraines during this period:(4)
Stress: This is a significant trigger for many individuals. Menopause can be a stressful time due to physiological and lifestyle changes, potentially leading to more frequent headache episodes.
Sleep disturbances: It's common for sleep patterns to be disrupted during menopause. Poor or insufficient sleep can not only trigger headaches but also exacerbate migraine symptoms.
Dietary triggers: Certain foods and beverages, like food additives, caffeine, and alcohol, can trigger headaches, especially migraines.
Dehydration: Inadequate fluid intake is a common headache trigger.
Can perimenopausal headaches feel different?
Research suggests that headaches during perimenopause may not follow a predictable pattern in some women. Unlike premenopausal and postmenopausal headaches, perimenopausal headaches can vary in frequency, severity, and type.
Hormonal fluctuations during this phase can make migraines worse for many women, especially those with a history of menstrual migraines. Studies indicate that the perimenopausal phase is associated with a higher frequency of migraines (≥10 headache days per month) than the premenopausal phase. However, migraine frequency tends to decline once women reach postmenopause, likely due to hormonal stabilization.(5)
Another notable difference is the increased likelihood of new-onset headaches during perimenopause. In a 2012 study, nearly 47.5% of women in this stage reported experiencing headaches they’ve never had before, while others noticed a worsening of preexisting headaches. Tension-type headaches (TTH) also become more common during this phase.(6)
However, not all women experience drastic changes. While some find their headaches worsening or shifting in type during perimenopause, others may notice little to no difference throughout the menopausal transition. Their headache patterns remain consistent, unaffected by hormonal fluctuations. This variability highlights the complex relationship between hormones and headaches, emphasizing the need for personalized management strategies.
Managing Headaches & Migraines During Menopause
An integrated approach is recommended to manage headaches. This may include HRT, medications for both prevention and acute treatment of headaches, and non-medicinal strategies. Experts suggest the following strategies to manage headaches and migraines:
Implementing Lifestyle Modifications
Women may want to make the following lifestyle changes during menopause to better cope with headaches and migraines.
Hydration: It’s important to drink plenty of water daily and aim for at least 1.5 to 2 liters to prevent dehydration, which is a common headache trigger.
Caffeine intake: Limiting consumption of coffee and energy drinks is advised, especially if they affect sleep.
Sleep: Maintaining a regular sleep schedule will improve sleep quality and reduce migraine frequency. This involves establishing a consistent bedtime and wake-up time every day.
Exercise: Engaging in moderate-intensity aerobic activities like walking or cycling for 30 to 50 minutes three to five times a week can help. Regular exercise can increase the levels of beta-endorphins in the body, which are known to improve moods and reduce stress and pain.
Diet: Eating regular meals throughout the day will maintain blood sugar levels. Choosing foods high in protein, fiber, and healthy fats and avoiding processed foods will help prevent migraines.
Stress management: Participating in activities that reduce stress and trying to avoid situations that increase it will help, as consistently managing stress is key to controlling migraine triggers.
Identifying and Avoiding Triggers
While specific foods such as red wine or caffeine can trigger migraine attacks for some individuals, not everyone is affected by food-related triggers. Keeping a headache diary is an effective strategy for identifying personal triggers. Individuals can detect patterns and pinpoint factors that may influence their symptoms by diligently tracking diet, stress levels, sleep patterns, and headache occurrences.
Using Pain Relievers
Some common options for pain relief include the following:
Nonprescription pain relievers: A nonsteroidal anti-inflammatory drug (NSAID), such as naproxen sodium (Aleve) or ibuprofen (Advil or Motrin) may relieve headaches as soon as they begin.
Triptans: These medicines block pain signals in the brain. Triptans often relieve headache pain within two hours. They also help control vomiting.(5,6)
Consider Hormone Replacement Therapy (HRT)
HRT can be an effective way to manage headaches and migraines for many women going through the menopausal transition. By stabilizing estrogen levels, HRT helps reduce the frequency and severity of these headaches and alleviate other common symptoms of menopause, like hot flashes.(5)
It’s crucial to consult a healthcare provider as they can tailor HRT to the specific needs of the individual. A doctor can prescribe the most effective dosage and method of administration to control headaches while also addressing the broader spectrum of menopausal symptoms.
Exploring Alternative Therapies
The following alternative options can also be effective in managing headaches and migraines:(7,8)
Acupuncture: This ancient Chinese practice involves the insertion of fine needles into specific body points, which is thought to activate the body's natural pain-relief mechanisms. Acupuncture may enhance blood flow and trigger the release of neurotransmitters that manage pain, potentially reducing the frequency and severity of migraine episodes.
Massage therapy: By targeting muscle stiffness and tension in the neck, shoulders, and back, massage therapy can alleviate the physical triggers of headaches. Regular massage sessions help relax these tension-prone areas and improve overall stress levels, reducing the likelihood of migraine occurrences.
Relaxation techniques: Engaging in practices such as mindfulness meditation, deep breathing exercises, and yoga can significantly lower stress, which is a common trigger for both tension headaches and migraines. These techniques foster a deep sense of relaxation and can improve the body's ability to cope with stress, leading to fewer and less intense headaches.
When to See a Doctor for Headaches During Menopause
Headaches that frequently occur or hamper quality of life should be evaluated by a healthcare professional. It’s important to seek immediate medical attention if experiencing any of the following symptoms:(4)
Sudden onset of severe headaches
Persistent headaches that worsen or do not improve with medication
A headache that is unusually intense or the first of its kind
Headaches severe enough to wake an individual from sleep
Headaches that occur with a high fever, rash, confusion, dizziness, or unexplained weight loss
Frequent headaches or migraines that disrupt daily activities
These signs could indicate underlying conditions that require diagnosis and treatment.
Experiencing headaches or migraines during menopause? Discover if HRT is right for you.
If you’ve entered the menopause transition and are struggling with headaches and migraines, you don’t have to suffer in silence. Take our brief menopause quiz to see if you’re an eligible candidate for HRT. Get started with Winona to take the first step toward feeling better.