Breakouts can be uncomfortable at any age. Pimples and other skin blemishes are often associated with puberty and adolescence, but the natural hormonal changes that take place during menopause can also make women more prone to breakouts. Research shows that one-third of doctor’s visits for acne cases involve women over the age of 25.(1)
Acne breakouts are one of the many changes the skin goes through during the menopause transition.(2) A number of factors, including oil production, bacteria, and inflammation, influence the development of acne.(3) Genetics, stress, sleep, physical activity, certain health conditions, and the use of makeup products are also known to play a role.(1)(4)
Breakouts in adulthood are more commonly seen in women than in men.(1)(5) Cases of adult female acne have also been increasing among perimenopausal and postmenopausal women. Breakouts may affect the whole face or be isolated around the chin or mouth region, particularly in postmenopausal acne.(1)(3)(5) Menopausal acne is categorized as new-onset, persistent, or recurrent.(1)(4) Some experts also use the term “late-onset acne.”(5) New-onset adult acne emerges in adulthood, while persistent acne develops during the teen years and continues into adulthood. Recurrent adult acne also starts in adolescence, clears up for a period of time, and then reappears later in adulthood. Of the three types, persistent adult acne is the most common among women.
Menopausal acne can lead to increased sensitivity, scarring, redness, and changes in skin pigmentation. Women experiencing menopausal acne may also be more prone to anxiety or depression, particularly if the blemishes are severe. Understanding why these breakouts develop and how to treat menopausal acne can help women achieve clear, healthy skin and enhance their quality of life.
When does menopausal acne occur?
Menopausal acne can develop during perimenopause, a period that typically lasts from two to eight years before menopause and up to one year after the final menstruation.(4) The perimenopausal stage can extend from mid-30s or late 30s to late 40s. Acne may also appear throughout menopause. Most women in the United States enter menopause around the age of 52.(6) Breakouts may present as small bumps (papules), fluid-filled pimples (pustules), larger nodules, or deeper cystic acne. Presently, more research is needed to fully understand the nature of menopausal acne.
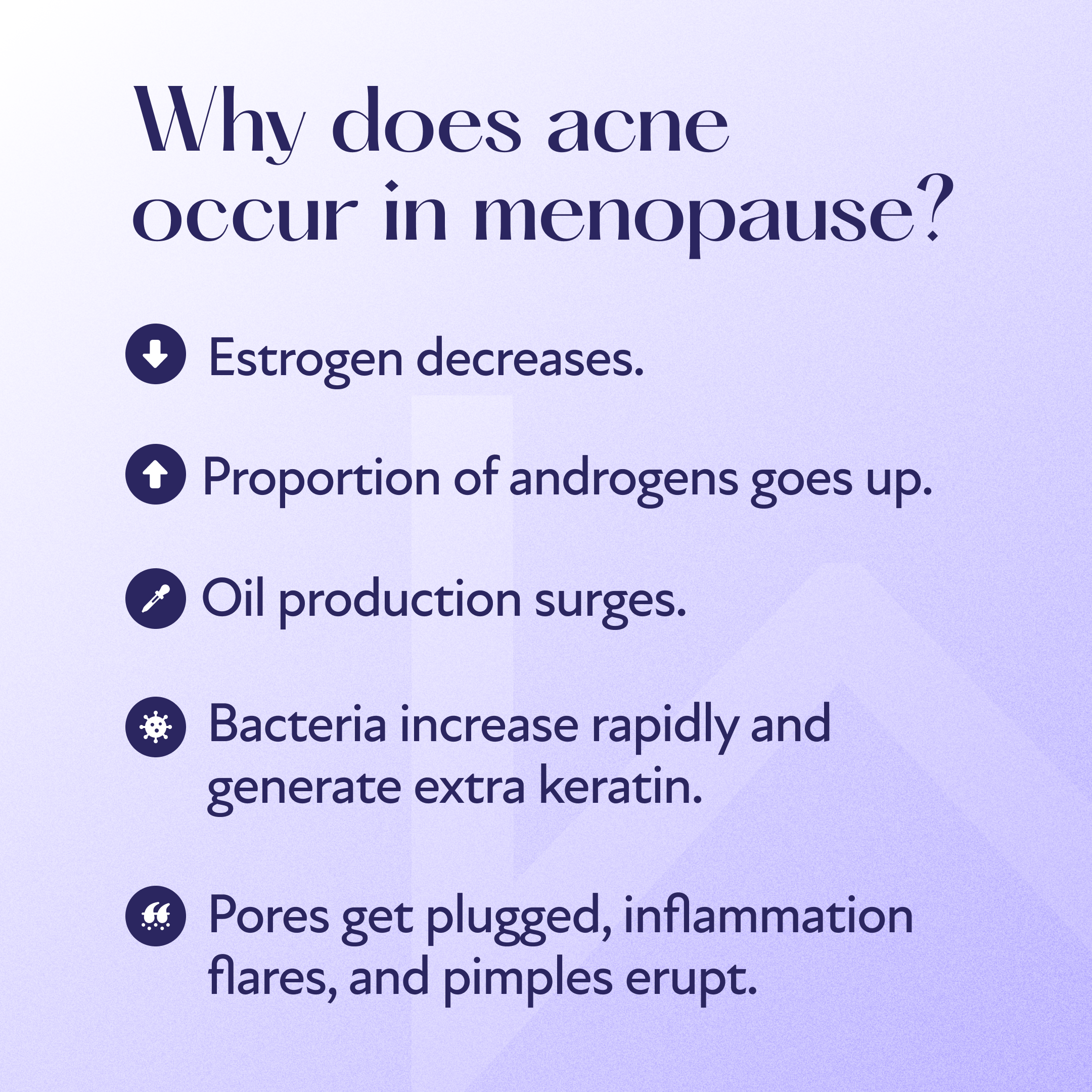
What causes menopausal acne?
Some of the main causes and contributing factors believed to influence the development of menopausal acne include the following:
Decreases in Estrogen: Although the underlying mechanisms behind menopausal acne are not entirely understood, changing hormone levels during menopause are believed to be the primary cause.(2) During this time, estrogen levels fall. The face is home to a large number of estrogen receptors, which influence the skin’s strength and elasticity.(5) As estrogen levels dip during menopause, the skin experiences a loss of collagen and hydration, along with an increase in wrinkles and sagging. All of these factors may contribute to the development of acne during menopause.
Increases in Androgens: Along with declining estrogen levels, androgen levels rise during the menopause transition. Androgens are a group of steroid hormones responsible for metabolism, regulating muscle mass, estrogen synthesis, the development of male secondary sexual characteristics, and more.(5)(7) These changes in androgen levels can stimulate oil production (sebum) in the skin and promote the growth of sebaceous glands, making women more prone to breakouts.
Stress: Stress during menopause may exacerbate skin problems. Increased stress is common during the menopause transition, with some research suggesting that women in early perimenopause may be particularly prone to stress, anxiety, or depression.(8) Chronic stress in adult women has been linked to elevated androgen levels and sebaceous hyperplasia, a condition characterized by the development of small bumps on the skin’s surface.(9)(10)
Genetics: Genetics may also influence menopausal acne, including the size and quantity of pimples, as well as the functioning of the skin’s oil glands.(11) Having a parent with adult acne makes a child more prone to the condition. Researchers suggest that women who are genetically susceptible to acne may experience flare-ups during perimenopause.(5)
Diet: During menopause, women experience hormonal changes that affect metabolism, appetite, and fullness. Certain foods may contribute to hormonal acne.(12) Experts explain that eating foods with a high glycemic index (GI), like sugary or processed foods, can cause blood sugar levels to rise. Elevated blood sugar promotes inflammation and increases sebum production.(13) These factors may be a recipe for breakouts in individuals prone to acne.
Symptoms of Menopause Acne
Women may experience different symptoms of menopausal acne. The size, location, and type of acne that develops can vary from one person to the next. Common signs of menopausal acne may include the following:(5)(14)
Small bumps, fluid-filled pimples, larger nodules, or deeper cysts on or below the skin
Pimples and blemishes on the face, particularly on the chin, around the mouth, or along the jawline
Pimples on the back, chest, or other areas of the body
Persistent or recurrent acne
How to Treat Menopausal Acne
Treating adult female acne and menopausal acne typically requires a multipronged approach. Treatment methods may vary based on factors like the underlying cause of the acne, its severity, skin sensitivity, lifestyle choices, medication use, and susceptibility to scarring. Here are a few remedies that may help prevent and manage menopausal acne:
A Gentle Skincare Routine: Developing a healthy skincare routine is particularly important during the menopause transition. Washing the face twice a day can help prevent acne breakouts. Experts recommend using gentle cleansers rather than harsh products that contain alcohol, which can irritate the skin.(15) Women are also advised to avoid rough facial scrubs. Instead, they should wet the face with warm water and softly massage cleanser into the skin using the fingertips, rinse with water, and lightly pat the skin dry with a soft towel. When it comes to face washing, more is not always better. Cleansing once in the morning and once before bedtime is optimal for healthy, clear skin. It’s also advisable to wash the face after excessive sweating.
Proper Moisturizing: Keeping skin hydrated is key to managing acne. Without enough moisture, skin can dry out, causing the body to ramp up oil production and increase the likelihood of acne. After washing the face, it’s important to apply a lightweight, non-comedogenic moisturizer that doesn’t contain oil and won’t clog pores or promote breakouts. Moisturizer can also be applied whenever skin feels tight or dry.
Topical or Oral Treatments: Certain over-the-counter (OTC) topical products can help target breakouts. These include gels and creams containing ingredients like benzoyl peroxide and salicylic acid.(5) Benzoyl peroxide eliminates bacteria, while salicylic acid helps unclog pores and minimize swelling and redness.(16)(17) In some cases, a doctor may prescribe antibiotics or recommend topical prescription treatments like tazarotene, tretinoin, or adapalene (adapalene may not always require a prescription).(1)(18) Patients with more severe cases of acne may be prescribed the oral medication isotretinoin. Individuals are encouraged to speak to a healthcare provider before starting any new medications.
Water-Based Makeup: Similar to choosing a non-comedogenic moisturizer, opting for water-based makeup products can help keep breakouts under control, as these skin-friendly cosmetics won’t block pores. Removing makeup at the end of the day is also essential for preventing acne, along with washing makeup brushes, which can harbor dirt and bacteria. Experts recommend thoroughly cleaning makeup brushes with shampoo once a week or every 10 days.(19)
Hormone Therapy: Hormone replacement therapy (HRT) is a natural treatment method that may help regulate hormones and improve symptoms of menopause. In addition to addressing night sweats, hot flashes, and mood changes, HRT may improve breakouts by restoring the hormonal balance that shifts during the menopause transition. Estrogen HRT, in particular, may boost collagen production, minimize oil secretion, and shrink sebaceous glands.(2) A doctor can help determine whether HRT may be a good fit for women going through menopause.
Treatment for adult acne can take time. While skin is healing, individuals should refrain from picking at blemishes, as this can irritate the skin and increase the risk of scarring.
When to See a Dermatologist for Menopausal Acne
Menopausal acne does not always require treatment. However, if breakouts are severe or do not improve with OTC treatments, individuals are encouraged to see a dermatologist. Some cases of adult acne may require stronger medications or alternative treatments.
In some instances, menopausal acne may be related to a health condition, such as a thyroid disorder or hyperandrogenism.(4) Hyperandrogenism, a defining characteristic of polycystic ovary syndrome (PCOS), occurs when a person has high levels of androgens in the body. Individuals with PCOS may experience irregular periods, excessive facial or body hair (hirsutism), ovarian growths, or acne.(20) If menopausal acne is accompanied by additional symptoms, individuals should consult a physician.
Struggling with acne during menopause? Discover if HRT is right for you.
If you’ve entered the menopause transition and are dealing with menopausal acne, you’re not alone. Take our brief menopause quiz to see if you’re an eligible candidate for HRT. Get started with Winona to take the first step toward feeling better.