Hormone replacement therapy (HRT) is the most effective treatment for managing menopausal symptoms such as hot flashes, night sweats, and vaginal dryness. While these symptoms often become milder after menopause, many women continue to experience them well into their later years. Studies show that vasomotor symptoms, like hot flashes, can persist for 7 to 12 years, and nearly half of women between 60 and 65 years of age still report symptoms.(1)
Many postmenopausal women also experience symptoms of genitourinary syndrome of menopause (GSM), a condition characterized by thinning, dryness, and inflammation of the vaginal and urinary tissues due to declining estrogen levels.
The postmenopausal phase is also a time when bone loss accelerates, increasing the risk of osteoporosis and fractures. As these health concerns and symptoms extend well beyond menopause, they raise an important question: Can HRT be taken safely after menopause?
The short answer is yes, HRT can be used after menopause, but it depends on several factors, including the age at which therapy is started, personal and family health history, and the presence of any risk factors such as cardiovascular disease or a history of breast cancer.
This article explores when and how HRT can be considered after menopause, the factors that influence this decision, and how a personalized approach can help women maintain their health, vitality, and quality of life well beyond menopause.

The Role of HRT After Menopause
Postmenopause begins after a woman has gone 12 consecutive months without a menstrual period. During this phase, the body produces much lower levels of estrogen and progesterone. These hormones are important for supporting many areas of health, and their decline can lead to symptoms such as hot flashes, night sweats, vaginal dryness, sleep disturbances, and mood changes. While some women experience only mild symptoms that improve over time, others continue to face persistent discomfort that affects daily life and overall well-being.(2)
HRT helps by replenishing the hormones that naturally decline after menopause. Restoring hormone levels can ease symptoms, support bone health, and improve quality of life after the menopausal transition.
It mainly involves either estrogen therapy alone (for women who have had a hysterectomy) or a combination of estrogen and progesterone (for women with an intact uterus). The addition of progesterone is important, as it helps protect the lining of the uterus from the risk of endometrial hyperplasia, a condition that can increase the chance of developing endometrial cancer.
The Benefits of HRT After Menopause
HRT helps manage vasomotor symptoms, supports vaginal health, and addresses other health problems that are common during and after the menopausal transition.(1)(3)(4)
Relief from Vasomotor Symptoms
One of the most immediate benefits of HRT is relief from vasomotor symptoms, such as hot flashes and night sweats. These symptoms can be exhausting, affecting sleep, mood, and quality of life. HRT remains the most effective treatment option for easing these symptoms and improving well-being.
Support for Vaginal and Urinary Health
HRT also addresses genitourinary syndrome of menopause (GSM), which includes symptoms such as vaginal dryness, discomfort during intimacy, and urinary issues. Restoring estrogen levels can improve vaginal health, ease irritation, and enhance comfort and quality of life.
Protection Against Bone Loss
Beyond symptom relief, HRT plays an important role in protecting bone health. After menopause, the decline in estrogen can lead to rapid bone loss, which increases the risk of osteoporosis and fractures. By helping to maintain bone density, HRT reduces the risk of fractures and supports overall strength and mobility.
Cardiovascular Benefits
Studies have shown that estrogen plays an important role in supporting heart health by managing cholesterol levels and maintaining the health of blood vessels. However, the heart-related benefits of HRT depend greatly on the timing of initiation. Research indicates that starting HRT within 10 years of menopause onset or before the age of 60 is associated with the most favorable cardiovascular outcomes.
Possible Support for Cognitive Health
Some research also suggests potential benefits of HRT for cognitive health. While more studies are needed, there’s growing interest in how HRT might help preserve memory and mental sharpness later in life.
Improvements in Skin Health
Estrogen plays a key role in maintaining skin elasticity, hydration, and thickness. Studies have shown that women on HRT experience improvements in skin texture and overall skin health compared to those who are not on HRT.
Risks and Side Effects of HRT After Menopause
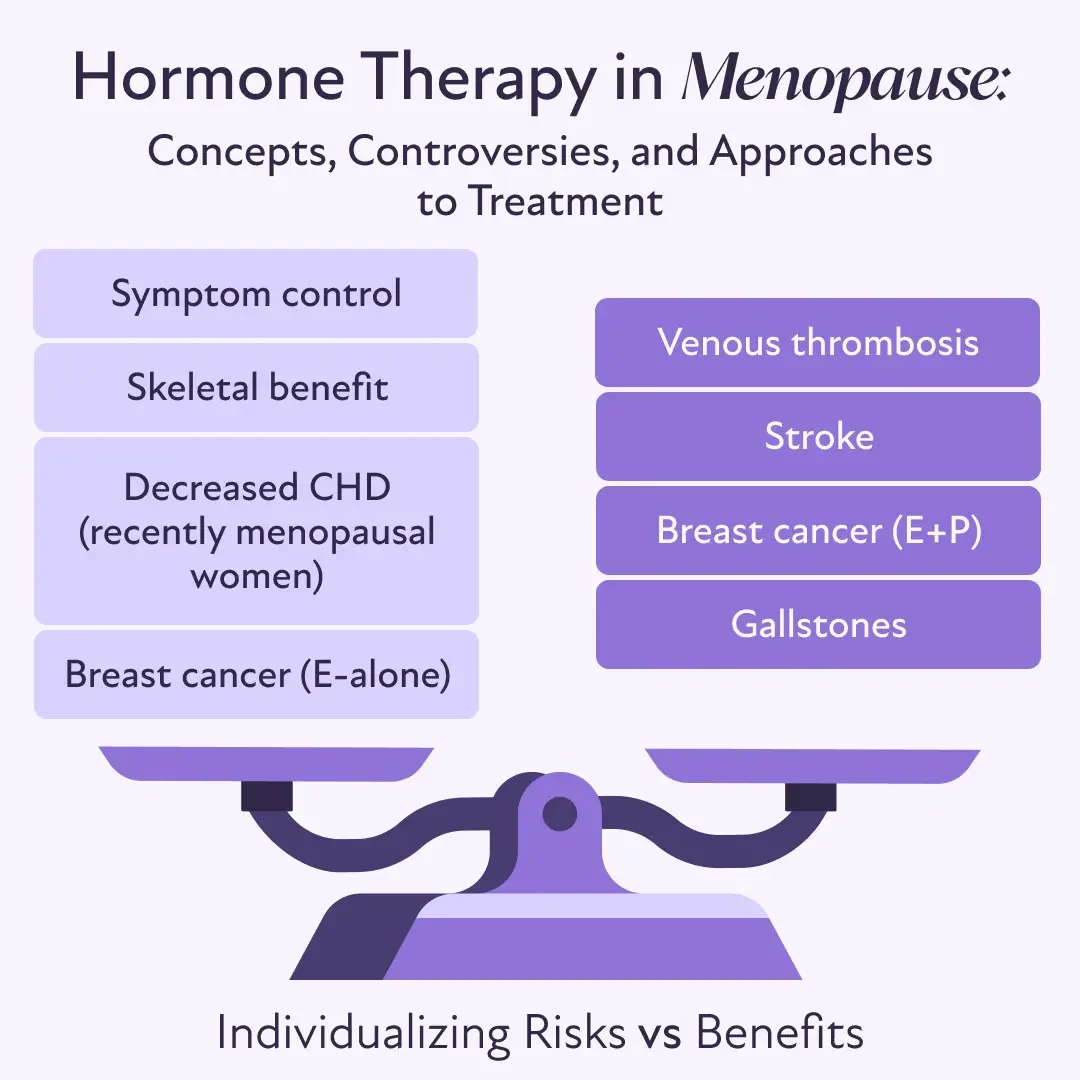
While hormone therapy can offer meaningful benefits, it’s important to approach treatment with a full understanding of the potential risks.(1)(3)(4)
Blood Clots and Stroke
One of the most discussed risks of HRT is an increased chance of developing blood clots, which can lead to serious conditions such as deep vein thrombosis (DVT). Some studies also suggest a slight increase in the risk of stroke. Opting for transdermal estrogen (delivered through a patch or cream) can lower this risk.
Breast Cancer
Another concern is the potential link between certain types of HRT and breast cancer. Studies have shown that synthetic progesterone may slightly increase breast cancer risk over time. However, not all hormone therapies carry the same level of risk. The type of progesterone used, the duration of therapy, and an individual's health history all play a role in determining the level of risk. Regular screening and personalized discussions with a healthcare provider can help monitor and manage this risk.
Impact on the Uterus and Bleeding Patterns
Women who still have a uterus need special consideration when using HRT. Estrogen alone can stimulate the uterine lining, increasing the risk of endometrial hyperplasia or even cancer. Adding progesterone helps protect against this risk. Some women may experience bleeding or spotting, especially when first starting therapy, but these side effects often settle over time. However, any unexpected or persistent bleeding should always be discussed with a healthcare provider.
Other Health Risks
Long-term use of HRT has been linked to slight increases in certain risks, including gallbladder disease. However, studies suggest that starting HRT earlier and using the lowest effective dose may offer more benefits than risks for many women. The specific formulation, dosage, and individual health factors all influence how therapy affects long-term outcomes.
Strategies to Minimize Risks
Mitigating risks begins with choosing the right therapy. A physician will carefully weigh the potential benefits and risks, taking into account each woman's personal and family health history. Transdermal or low-dose options tend to offer a better safety profile compared to higher-dose oral formulations. Individualized care remains essential. A woman’s symptoms, overall health, and long-term goals should guide the selection of therapy. Regular follow-up visits with a healthcare provider allow for ongoing monitoring and timely adjustments and ensure that treatment continues to support changing health needs over time.
When and How to Start HRT After Menopause
Research shows that starting HRT within 10 years of menopause or before the age of 60 often brings the greatest benefits with a lower risk of complications. Early use has been associated with improvements in heart health, bone density, and overall well-being.
However, these general guidelines are not one-size-fits-all. A woman’s personal health history plays a critical role in determining whether HRT is the right choice. Even among women younger than 60, a history of certain conditions, such as heart disease, stroke, blood clots, breast cancer, or liver disease, may increase the risk of side effects.
Before starting therapy, it’s important to have a thorough evaluation of personal risk factors. This includes not only medical history but also lifestyle habits, like smoking and physical activity, as well as family history of disease. In some cases, a different formulation, lower dose, or nonhormonal treatment may be a safer alternative.
Deciding when and how to start HRT should always be a collaborative decision between a woman and her healthcare provider. By carefully weighing the benefits and risks, a personalized plan can be developed that supports symptom relief, protects long-term health, and respects each woman’s unique situation.
Personalized Approaches to HRT After 60 or 65
Most experts do not recommend starting HRT for the first time after the age of 60. This is because starting later may carry a higher risk of complications, especially for women with existing health conditions. However, for women who have already been using HRT and continue to benefit from it, a personalized approach becomes essential.
Each woman’s health history — such as a history of heart disease, cancer risk, blood clots, or lifestyle factors like smoking and exercise — plays a critical role in shaping the safest and most effective HRT plan. In some cases, adjusting the type, dose, or method of HRT can make a significant difference in outcomes.
A 2024 study published in Menopause: The Journal of the Menopause Society found that continuing low-dose transdermal or vaginal hormone therapies after age 65 may lower the risk of mortality, heart disease, dementia, and even some cancers. Estradiol-based therapies appeared especially beneficial compared to conjugated estrogens.(5)
Major organizations like the American College of Obstetricians and Gynecologists (ACOG) also advise against routinely discontinuing systemic estrogen at age 65. Instead, they recommend that decisions be based on symptoms, overall health status, and personal goals. Some women may choose to continue therapy, while others may find it helpful to reduce the dose or switch to a different formulation.
The average woman is on HRT for 5 years, but it’s safe to take HRT for as long as needed to treat symptoms. We generally suggest a trial period going off the medications after 2-3 years of use. If a patient feels fine without the HRT, it’s time to stop taking it. If the symptoms return, they can con

Personalized care remains the cornerstone. With the right guidance, women over 60 can still enjoy the quality-of-life benefits of HRT while minimizing potential risks.
Other Treatment Approaches
Individuals can also consider non-medical and complementary strategies to help manage symptoms and support long-term health.(6)
Lifestyle Changes
Dressing in layers that are easy to remove during hot flashes
Keeping a fan nearby and maintaining a cool ambient temperature, especially at night
Avoiding hot drinks, spicy foods, caffeine, and alcohol to minimize triggers
Using an ice pack under the pillow for quick cooling relief
Quitting smoking and limiting alcohol consumption to reduce the severity of vasomotor symptoms
Exercising regularly with activities like brisk walking or light weight training to potentially shorten symptom duration and benefit heart and bone health
Stress Management and Relaxation Techniques
Practicing deep breathing exercises and stretching may help lower the intensity of hot flashes.
Incorporating yoga and meditation can help manage stress and support emotional well-being.
Focusing on relaxation techniques may reduce symptom frequency by calming the nervous system.
Vaginal Health Support
Using nonhormonal vaginal moisturizers regularly to relieve dryness
Applying lubricants during sexual activity to reduce irritation and discomfort
Maintaining regular sexual activity, which may help improve vaginal blood flow and tissue health
Nonhormonal Medications
For women who cannot or prefer not to use hormone therapy, several nonhormonal medications have been shown to help manage menopausal symptoms, especially hot flashes and night sweats.(6)
Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): These antidepressants, such as paroxetine, can significantly reduce the frequency and severity of hot flashes. They also offer the added benefit of supporting mood and reducing anxiety, which are common concerns during menopause.
Fezolinetant: This is a selective neurokinin-3 receptor (NK3R) antagonist. It works by blocking specific brain signals that trigger hot flashes, helping to lower their frequency and intensity without affecting hormone levels.
Clonidine: Originally used as a blood pressure medication, clonidine can help expand the body's thermoneutral zone, stabilizing body temperature regulation and resulting in a reduction in the frequency and severity of hot flashes.
Making the Decision to Start or Continue HRT After Menopause
Choosing whether to start or continue HRT after menopause is a personal decision that requires balancing the benefits and risks. HRT can relieve vasomotor symptoms, protect bone health, and support genitourinary health, but longer use may increase the risk of breast cancer, blood clots, stroke, or heart disease. Women who begin HRT closer to menopause often continue to benefit over time, whereas those starting more than a decade after menopause need careful evaluation and medical guidance.
Regular follow-ups are essential for monitoring symptoms, reassessing risks, and adjusting treatment as needed. With the right approach, whether it involves modifying the dose, switching formulations, or tapering off, HRT can continue to support long-term health and quality of life, always guided by shared decision-making between women and their healthcare providers.