Women are nearly twice as likely as men to develop depression, a disparity that has prompted researchers to investigate the role hormones play in mood regulation.(1) Studies suggest that the brain’s structure and function can change in response to fluctuating ovarian hormones, increasing vulnerability to mood disorders.(1)
This article explores how fluctuations in hormones, like estrogen and progesterone, can impact emotional health and suggests treatment options for a better hormonal transition.
Can hormonal imbalance cause depression?
While not all women experience depression during periods of hormonal fluctuations, there is substantial evidence that indicates hormonal imbalances can contribute to mood disorders.
A study highlights how natural changes in hormone levels can affect brain morphology and neurochemistry.(2) Hormonal shifts can disrupt the balance of neurotransmitters — chemicals that allow communication between nerve cells — leading to mood imbalances.
These changes in neurotransmitters can affect brain regions involved in emotional processing, like the cortico-limbic structures, increasing vulnerability to depression and anxiety.(2)
Fluctuations in hormone levels may also cause structural changes in the brain. Studies suggest that these fluctuations can contribute to a reduction in gray matter volume (a key component of the brain's nerve tissue), causing mood changes. These changes are particularly evident in the hippocampus, a brain area crucial for memory and mood regulation, further contributing to emotional disturbances.(2)
These findings suggest that the natural ebb and flow of reproductive hormones across different life stages can influence mood and increase the risk of depression, particularly during significant hormonal transitions like puberty, pregnancy, and menopause.
What Hormones Cause Depression?
Estrogen and progesterone likely contribute to depression through their impact on key neurotransmitters and brain functions that regulate mood. Estrogen, in particular, has been shown to influence serotonin, a neurotransmitter crucial for maintaining emotional stability. Decreased serotonin activity, often seen during periods of low estrogen, has been linked to a higher vulnerability to mood disorders like depression.(2)
Dopamine, known as the "reward neurotransmitter," plays a significant role in regulating mood, motivation, and pleasure. Estrogen helps maintain dopamine levels by reducing its breakdown and reuptake, thus supporting emotional well-being.(2)
Progesterone, alongside estrogen, can also influence dopamine activity, depending on the brain region. For instance, in the nucleus accumbens (a brain region that influences behaviors), progesterone boosts dopamine release, which may reduce depressive symptoms. However, in the prefrontal cortex (the area responsible for decision-making), it can inhibit dopamine, potentially affecting emotional regulation.(2)
Progesterone and estrogen can also interact with gamma-aminobutyric acid (GABA) receptors through allopregnanolone, a brain steroid derived from progesterone. Preclinical studies have shown that this interaction with GABA receptors has antidepressant properties, producing a calming effect and positively influencing mood regulation.(2)
The influence of these hormones also extends to energy production in the brain tissues, with estrogen playing a key role in regulating genes responsible for metabolism and energy production within cells. This impact on cellular energy can further affect overall brain function and mood.(2)
Below are other hormones that can contribute to depression:
Testosterone: Lower levels of testosterone, particularly in women during menopause, can result in fatigue, reduced motivation, and symptoms of depression.(3)
Thyroid hormones: An underactive thyroid (hypothyroidism) often causes fatigue, low mood, and depression, while an overactive thyroid (hyperthyroidism) may lead to anxiety and restlessness.(4)
Cortisol: Known as the stress hormone, cortisol helps the body respond to stress and maintain energy throughout the day. Chronic stress can lead to elevated cortisol levels, which are often associated with increased anxiety, weight gain, and depressive symptoms.(5)
Hormonal Depression During Various Life Stages
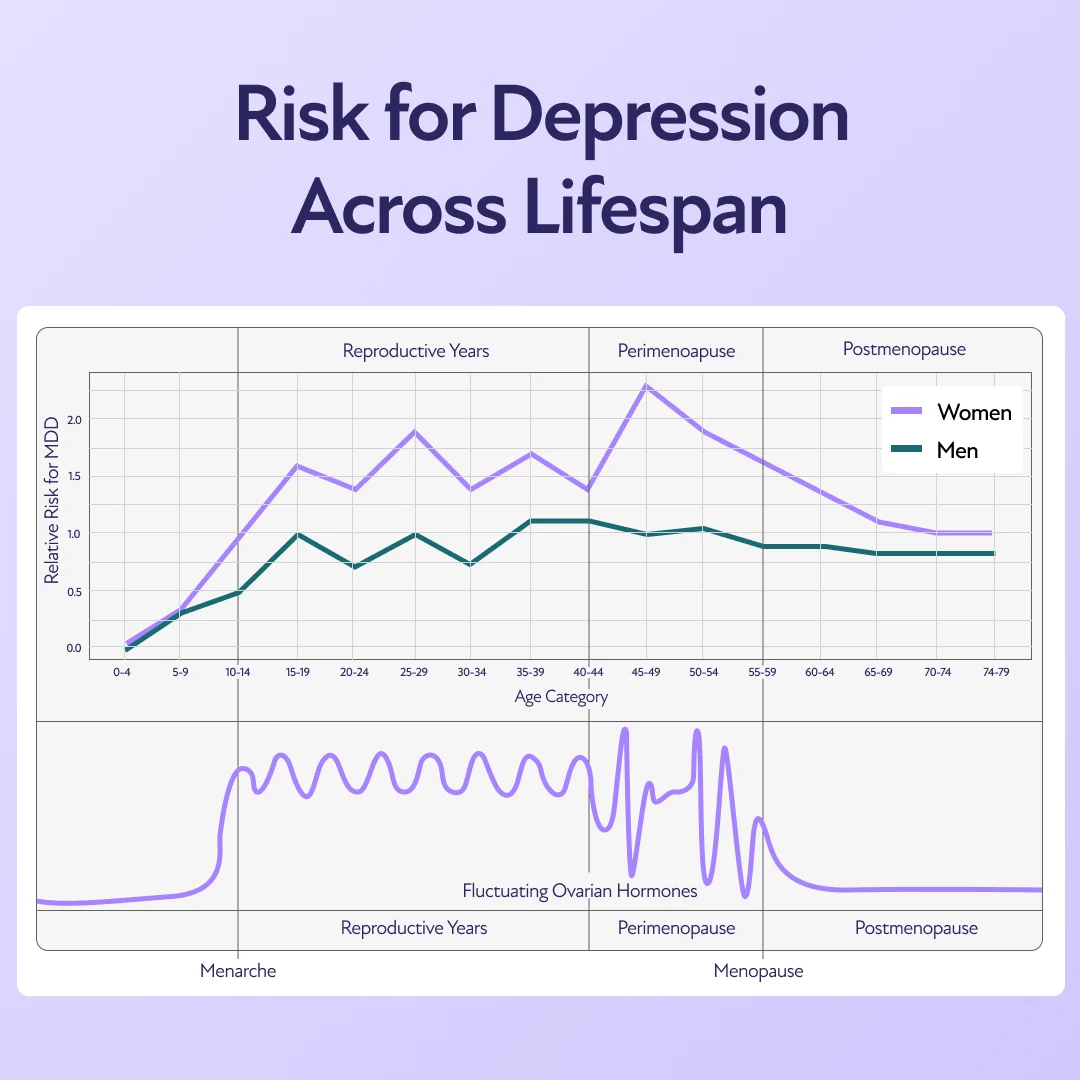
Hormonal changes during the menstrual cycle, pregnancy, and menopause can affect mental health.
Menstruation
A Harvard study on moods and menstrual cycles found that women between the ages of 36 and 45 with lower levels of estrogen and higher levels of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) were more likely to have experienced episodes of depression.(2)
These hormonal fluctuations during the premenstrual period, particularly in the late luteal phase, can lead to mood disturbances, especially in women with premenstrual dysphoric disorder (PMDD).
PMDD is a severe form of premenstrual syndrome (PMS) that affects emotional well-being and involves intense symptoms like mood swings, irritability, and depression. Unlike PMS, which typically causes mild discomfort, PMDD can significantly impact daily life, with symptoms appearing in the last 7–10 days of the menstrual cycle.(6)(7)
Women with PMDD are particularly sensitive to shifts in estrogen and progesterone during this phase. Higher levels of sex hormone binding globulin (SHBG) can further reduce the availability of estrogen, potentially worsening mood-related symptoms.(6)
Postpartum
Postpartum depression (PPD) is closely tied to the significant hormonal changes that occur after childbirth. One key hormone involved is allopregnanolone, a neurosteroid produced from progesterone.(8) During pregnancy, allopregnanolone levels steadily rise and peak in the third trimester. After childbirth, these levels drop rapidly, which can trigger depressive symptoms. While allopregnanolone levels usually recover within a few days after delivery, some women experience delayed recovery, increasing the risk of postpartum depression.
Additionally, GABA receptors, which help regulate mood, are affected by hormonal shifts, particularly changes in allopregnanolone. This disruption in GABA receptor function may contribute to the mood disturbances seen in postpartum depression.(8)
Research supports the link between hormonal changes and PPD. In a study, researchers induced low hormone levels in women with a history of postpartum depression, then provided hormone replacement and later withdrew it. After stopping the hormones, 63% of the women with a history of postpartum depression developed significant depressive symptoms, while none in the control group did.(9) These results suggest that hormonal changes during the postpartum period can trigger depression, especially in women already at risk.
Menopause
Fluctuating estrogen levels during perimenopause can alter brain chemicals like serotonin and dopamine, which help regulate mood. These changes in brain chemistry can predispose individuals to depression, making emotional regulation more challenging.
At the same time, DHEA levels, which serve as precursors to estrogen and testosterone, also decline. This drop in DHEA, combined with fluctuating estrogen levels, may further increase the risk of depression, adding another layer of hormonal imbalance.(10)
Additionally, lower estrogen levels often cause vasomotor symptoms, such as hot flashes and night sweats, which can disrupt sleep. Poor sleep can contribute to mood changes, creating a cycle where lack of rest intensifies the emotional impact of perimenopause.(11)

How to Treat Hormonal Depression
Consulting a psychiatrist can be an important first step in addressing hormonal depression, as they can provide guidance on the best treatment options based on an individual's specific needs. In many cases, a combination of approaches is most effective in managing symptoms. Here are a few options commonly recommended:
Hormone Replacement Therapy (HRT): HRT can help stabilize estrogen and progesterone levels, potentially easing mood swings and depression. Research has demonstrated that women using estrogen or combined hormone replacement therapy (HRT) saw a 68%–80% improvement in their depressive symptoms, while only 20%–23% of women not on HRT experienced similar improvements.(12) However, the effectiveness of HRT can vary, and it’s often used alongside other treatments.
Antidepressants: These medications help balance neurotransmitters that regulate mood and can be used alone or in combination with HRT, depending on the individual's hormonal and mental health needs.(13)
Therapy: Cognitive behavioral therapy (CBT) is widely recognized as one of the most effective treatments for depression. It helps individuals pinpoint and reshape negative thought patterns that impact emotions. By promoting more balanced thinking, CBT equips people to handle stressful situations more effectively, reducing the feeling of being overwhelmed.(14)
Dietary Changes: Maintaining a nutritious and balanced diet that is low in sugar and processed foods can help improve overall health and ease depressive symptoms. A diet rich in fruits, vegetables, lean proteins, and whole grains supports both mental and physical well-being.(15)
Regular Exercise: Physical activity is a proven way to boost mood and reduce symptoms of depression. A 2015 study showed that regular exercise, particularly aerobic activities, can raise endorphin levels, helping to improve mood and overall mental health.(16)
Stress Management: Incorporating stress-relief practices such as yoga, meditation, or engaging in hobbies can help ease the emotional burden that comes with hormonal changes. Managing stress can improve mental clarity and emotional balance.
Natural Remedies for Hormonal Depression
When considering natural remedies for depression, some individuals explore options like ginseng, red clover, and evening primrose oil. These supplements are commonly used to help manage symptoms related to hormonal imbalances. However, it's important to note that research on their effectiveness is limited and mixed. As with any treatment, it’s crucial to consult with a healthcare professional before adding these to your routine to ensure they are safe and appropriate for your specific needs.
Overcoming Emotional Challenges of Hormonal Depression
Hormonal depression can significantly impact emotional well-being during various life stages. From lifestyle modifications and therapy to hormone replacement therapy and antidepressants, a combination of tailored approaches can help women navigate these challenges and improve their quality of life. Taking proactive steps to manage hormonal transitions can empower women to regain emotional balance and overall health.